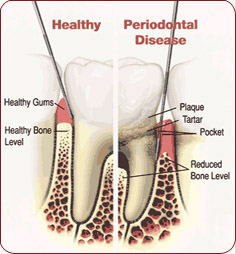
 Gingivitis is a type of gum disease; although it is not especially severe, it can lead to periodontitis if it is not treated. With this more advanced type of gum disease, “gums pull away from the teeth and form spaces (called ‘pockets’) that become infected. The body’s immune system fights the bacteria as the plaque spreads and grows below the gum line.” Unfortunately, this leads to additional problems: “Bacterial toxins and the body’s natural response to infection start to break down the bone and connective tissue that hold teeth in place.” Ultimately, the problem may result in removal of the teeth: “If not treated, the bones, gums, and tissue that support the teeth are destroyed. The teeth may eventually become loose and have to be removed.”
Gingivitis is a type of gum disease; although it is not especially severe, it can lead to periodontitis if it is not treated. With this more advanced type of gum disease, “gums pull away from the teeth and form spaces (called ‘pockets’) that become infected. The body’s immune system fights the bacteria as the plaque spreads and grows below the gum line.” Unfortunately, this leads to additional problems: “Bacterial toxins and the body’s natural response to infection start to break down the bone and connective tissue that hold teeth in place.” Ultimately, the problem may result in removal of the teeth: “If not treated, the bones, gums, and tissue that support the teeth are destroyed. The teeth may eventually become loose and have to be removed.”
Many people assume that all is well if they have no pain or obvious discomfort; however, the American Dental Hygienists’ Association (ADHA) notes that gingivitis can be painless in the early stages. There are some red flags that may indicate the presence of gingivitis; it is important to be aware of them and begin treatment before the disease progresses. Symptoms can include chronic bad breath, gums that are red and/or swollen, gums that are sore or prone to bleeding, and pain when chewing food. In addition, teeth may be sensitive and may become loose; finally, gums may appear to have gotten smaller and teeth may consequently appear larger.
How is gingivitis treated?
The type and scope of the treatment will depend on the extent of the gum disease; in addition to deep cleaning methods of treatment, there are also surgical and medicinal treatments. In some cases, gingivitis may be treated with some combination of these treatment options. Although some of the treatment will happen in the dentist’s office, “Any type of treatment requires that the patient keep up good daily care at home. The doctor may also suggest changing certain behaviors, such as quitting smoking, as a way to improve treatment outcome.”
Gingivitis is preventable
Rather than dealing with gingivitis – and even periodontitis – it is advisable to practice the best possible oral care and visit the dentist on a regular basis to keep gingivitis at bay and detect it early if it develops. The American Dental Hygienists’ Association recommends regular visits “every six months or as scheduled by your dental hygienist.”
Finally, it is important to note that gingivitis and periodontitis can be a problem during pregnancy. According to the ADHA, hormonal changes are partly to blame. “When gingivitis is evident, both the dental hygienist and the pregnant patient should make every effort to reverse or control the progress of the disease. One of the first things that should be discussed with the expectant mother is proper brushing and flossing techniques.” In addition, if the patient is vomiting as a result of morning sickness, the ADHA notes that she “should be advised to rinse the mouth with water and then brush her teeth to neutralize the acid. It may also be beneficial to suggest a well-balanced diet including plenty of vitamins C and B 12.” This is essential because periodontitis can compromise the baby’s health and well-being.
As always, if you have questions or specific concerns, Moore Family Dental would be happy to help!



